- INSPIRE Clinical Case Studies
Reducing Invasive Ventilation Days for Babies by Introducing NeoFlow® Delivery Room CPAP
- Product Featured: NeoFlow®

Background
As part of a quality improvement project, we aimed to reduce the number of intubations we were performing at delivery because evidence shows that doing so and stabilising babies on CPAP at birth reduces death and chronic lung disease.
Problem or Challenge
Pressure on the trigemino-cardiac nerve by the face mask during delivery of PEEP has been shown to result in apnoea and bradycardia in up to 50% of infants. It is also difficult to maintain continuous PEEP during transfer from the labour ward to the neonatal unit.
At our unit in Coventry, we sought a solution to combat these difficulties and maintain effective PEEP within the delivery room, during delivery room cuddles and on transfer to the neonatal unit.
Solution
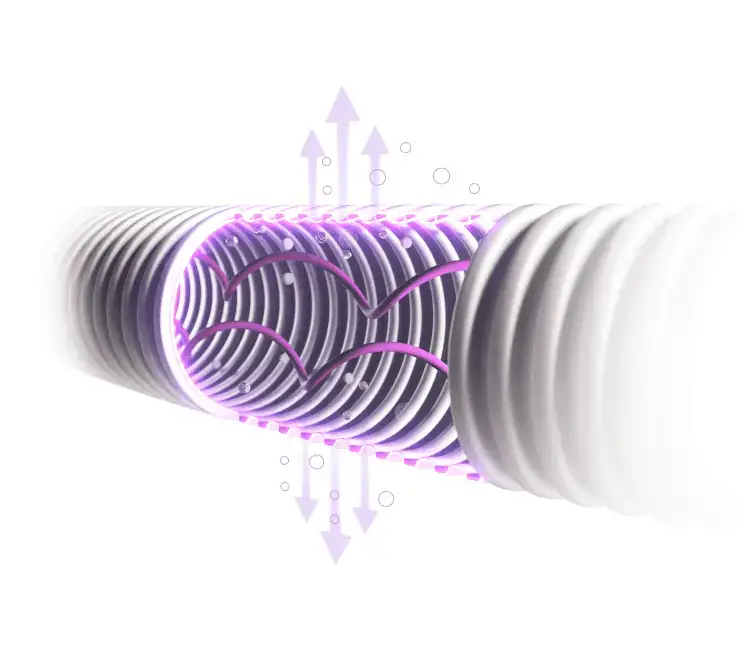
The NeoFlow® delivery room CPAP circuit enabled us to deliver continuous nasal CPAP through the resuscitaire without the need to purchase expensive additional equipment.
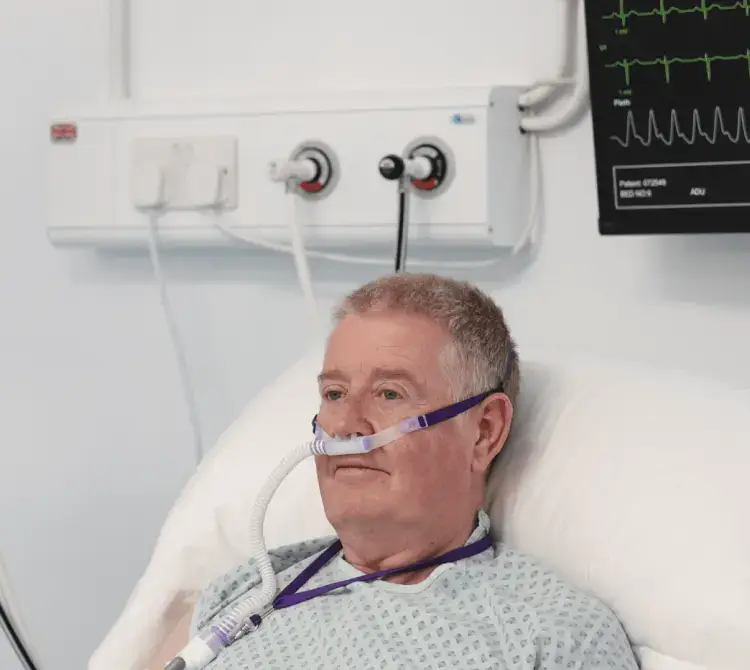
We adopted the circuit and developed an accompanying algorithm guiding the practitioner to deliver uninterrupted PEEP in the delivery room through to admission on the neonatal unit, using nasal mask or prongs.
Team consensus agreement was to use DRCPAP in babies born at or less than 30 weeks gestational age, and for all these babies regardless of gestation to be assessed individually and its use considered.
We set these criteria to focus on the cohort of babies most at risk of chronic lung disease and optimise our lung protective strategies.
A major benefit of this circuit is the long distal attachment which makes it possible for DRCPAP to be applied during optimal cord clamping and delivery room cuddles.
It also quickly and easily converts into a Tom-thumb circuit should conventional face mask ventilation be required.
Benefits and Outcomes
This initiative along with implementation of a respiratory care bundle has led to a reduction in the total number of invasive ventilation days for babies at Coventry along with a decrease in the incidence of chronic lung disease. We have also demonstrated that most babies between 24-27 weeks gestation and/or >600g can be safely stabilised using delivery room CPAP as the initial mode of breathing support.
It is also now routine practice to offer delivery room cuddles to parents on both labour ward and in theatres because of the ease of maintaining breathing support with this circuit.
Download Case Study
Latest Case Studies

Profile
University Hospitals Coventry and Warwickshire
Lucy Bradley
Advanced Neonatal Nurse Practitioner
Neonatal Unit