Home > High Flow Oxygen Therapy
High Flow Oxygen Therapy
High Flow Oxygen Therapy
What is High Flow Oxygen Therapy?
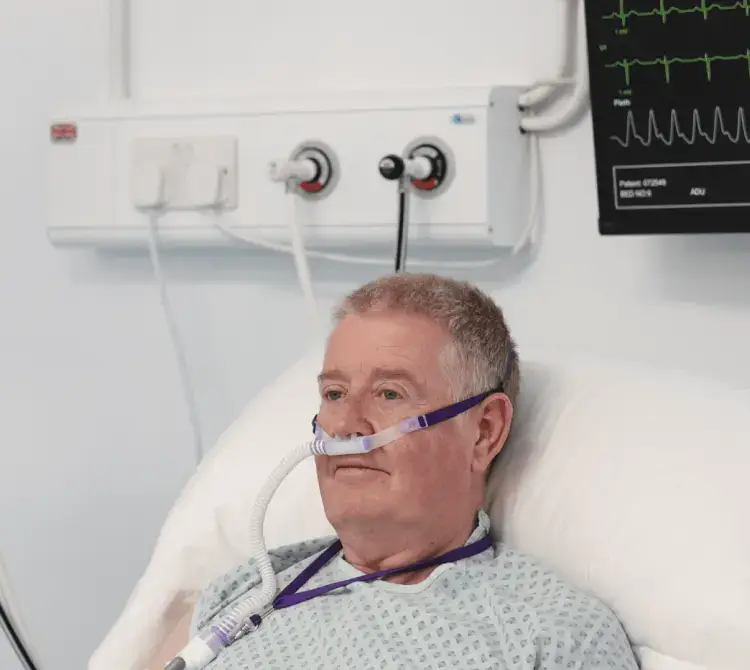
High-flow oxygen therapy is non-invasive respiratory support that delivers warmed, humidified, oxygen-enriched air to patients at flows to help meet and exceed their peak inspiratory demand. This is predominately by way of a nasal cannula which can provide warmed and humidified airflows as high as 80l/min and FiO2 of 21- 100%. Benefits of high flow are both clinical and physiological. The use of a high-flow nasal cannula is often associated with a prolonged expiration through a resistive effect that reduces the respiratory rate. This method may also assist in mucociliary clearance of secretions through humidified gas, is easy to apply, may improve patient comfort and improve alveolar ventilation [1,2].
Benefits include – Patient comfort and reduction in work of breathing, improvement in oxygenation and increased alveolar ventilation.

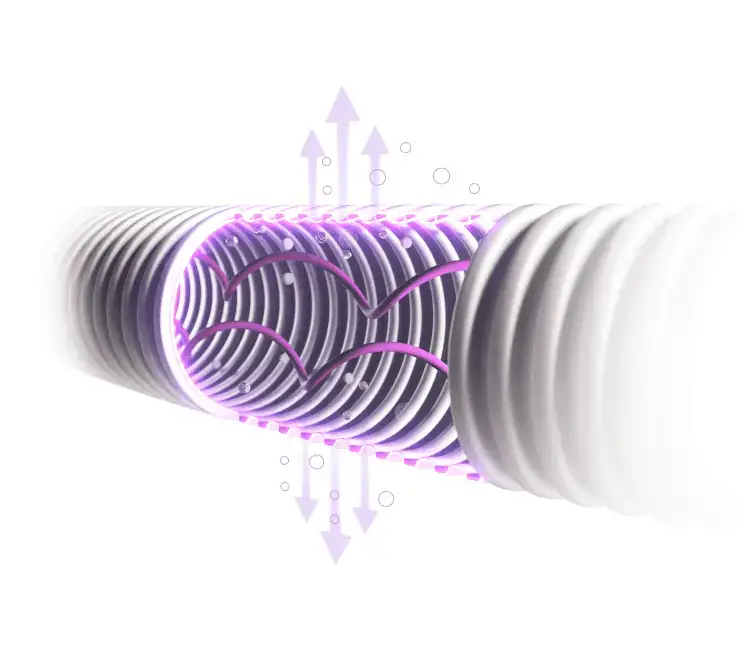
Improved Mucociliary Clearance
Improves mucociliary clearance with heated and humidified gases, enhances patient comfort and tolerance [1-5]
Variable Level of PEEP
Variable level of PEEP in upper airways can facilitate alveolar recruitment [6,7]
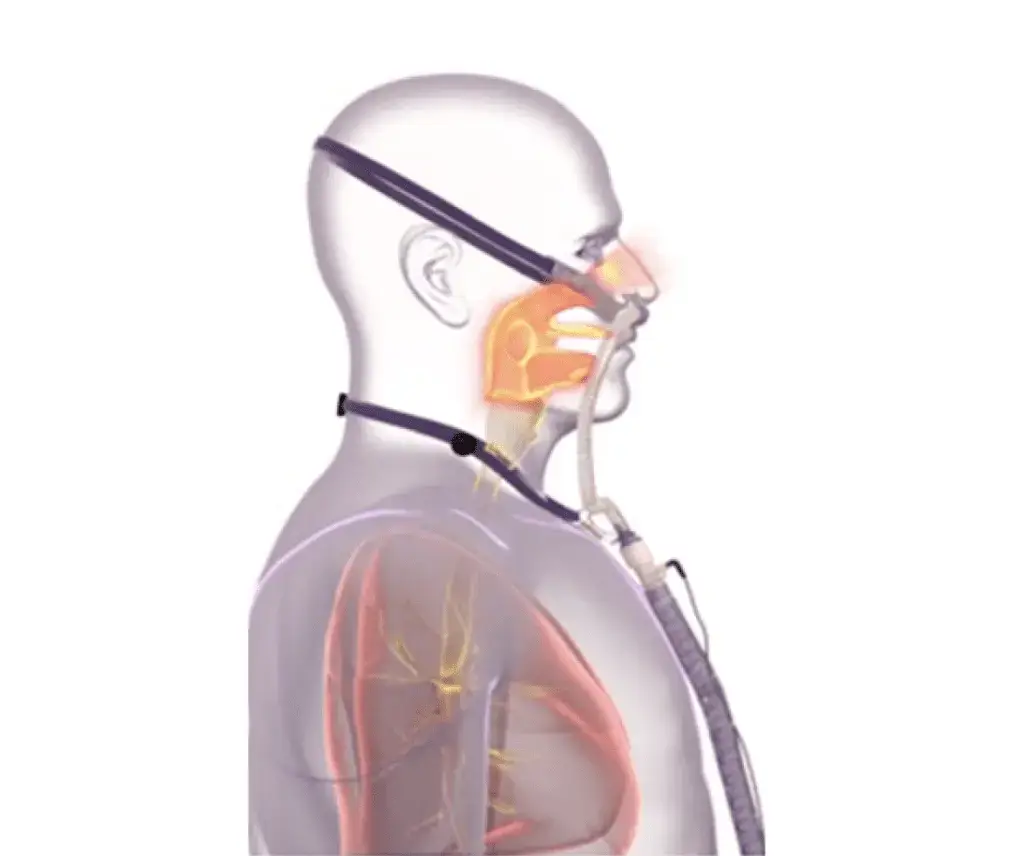
Reduction of Dead Space
Reduction of dead space through wash-out resulting in reduced co2 rebreathing and improved alveolar ventilation [8,9]
Frequently Asked Questions
What are the current guidelines for the use of HFOT?
It is typically used for spontaneously breathing patients who require oxygen at higher flow rates. High-flow oxygen therapy can effectively be used to treat patients with mild to moderate levels of hypoxemic respiratory failure [10]. The European Respiratory Society conditionally recommend the use of HFOT over conventional oxygen with acute hypoxemic respiratory failure, likely benefiting patients that are a high risk of intubation [10]. There are also conditional recommendations from the American Association for Respiratory Care that HFOT may reduce the need for invasive ventilation due to its effects on oxygenation and reduce risk of reintubation when used immediately post extubation [11]
As compared with conventional oxygen therapy, the application of high-flow nasal cannula immediately after extubation has been successful in preventing reintubation in certain high-risk populations, such as patients with COPD, coexisting cardiac conditions, or obesity [12]
What role does humidification play in HFOT?
Mucociliary clearance, effected by the coordinated beating of cilia, is the first line of defence to maintain pulmonary health and is responsible for clearing both the upper (nasal cavity) and lower airways of mucus, particulate matter, and pathogens.
Williams et al. described a range of dysfunction that can occur in the respiratory tract if the humidity and temperature of the delivered gas to a patient are not optimal [13]. These include thickened mucus, causing mucociliary transport to slow or stop, reduced ciliary movement and decreased lung compliance, and reducing functional residual capacity which can lead to atelectasis and shunting [14]
Furthermore, Fontanari and colleagues showed that receptors in the nasal mucosa respond to cold and dry gas to elicit a protective bronchoconstrictor response in both normal subjects and asthmatics [15,16]
Properly conditioned gas provides for patient comfort and minimizes deterioration of nasopharyngeal structures, improves lung and airway mechanics by eliminating the effects of drying/cooling [17]
What are the recommended starting flow rates for High Flow Oxygen?
Clearance of dead space has been suggested as being the key mechanism of respiratory support with NHF therapy. NHF clears the upper airways of expired air, which reduces dead space by a decrease of rebreathing making ventilation more efficient. The dead space clearance is flow and time dependent. Moller et al reported that the airway anatomical dead space where gas exchange does not occur is approximately 150ml. Using high flow oxygen, with flows greater than 45lpm in adult patients, we can reduce the anatomical dead space by 1 third which means greater clearance of CO2 and reduced CO2 rebreathing [18]
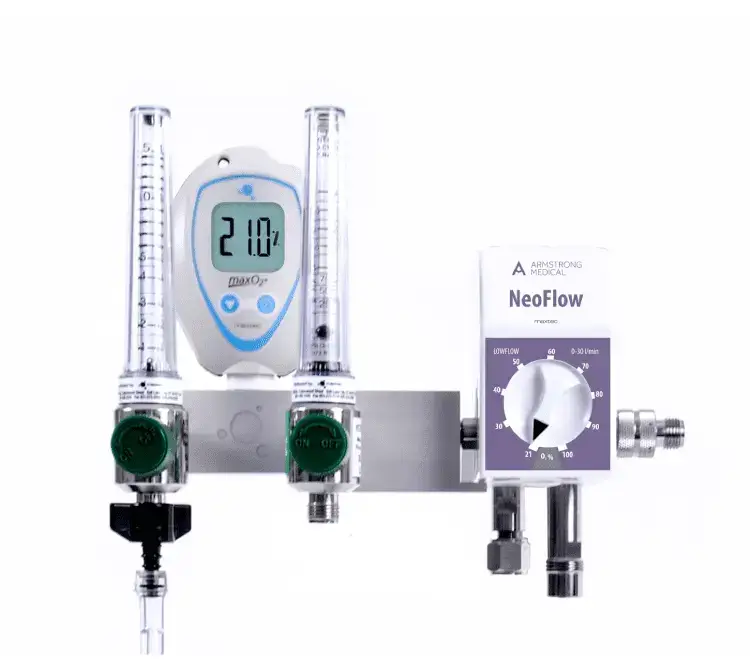
Dual Therapy Flow Driver - CPAP & HFOT
HFOT Products
References
[1] Munshi L, Mancebo J, Brochard LJ. Noninvasive Respiratory Support for Adults with Acute Respiratory Failure. N Engl J Med. 2022 Nov 3;387(18):1688-1698. doi: 10.1056/NEJMra2204556. PMID: 36322846.
[2] Elise Cuquemelle, Tai Pham, Jean-François Papon, Bruno Louis, Pierre-Eric Danin, Laurent Brochard. Heated and Humidified High-Flow Oxygen Therapy Reduces Discomfort During Hypoxemic Respiratory Failure. Respiratory Care Oct 2012, 57 (10) 1571-1577; DOI: 10.4187/respcare.01681
[3] Chidekel A, Zhu Y, Wang J, et al. The effects of gas humidification with high-flow nasal cannula on cultured human airway epithelial cells. Pulm Med 2012; 2012: 380686.
[4] Papazian L, Corley A, Hess D, et al. Use of high-flow nasal cannula oxygenation in ICU adults: a narrative review. Intensive Care Med 2016; 42: 1336–1349
[5] Cortegiani A, Crimi C, Noto A, et al. Effect of high-flow nasal therapy on dyspnea, comfort, and respiratory rate. Crit Care 2019; 23: 201.
[6] Frat JP, Thille AW, Mercat A, Girault C, Ragot S, Perbet S, Prat G, Boulain T, Morawiec E, Cottereau A, Devaquet J, Nseir S, Razazi K, Mira JP, Argaud L, Chakarian JC, Ricard JD, Wittebole X, Chevalier S, Herbland A, Fartoukh M, Constantin JM, Tonnelier JM, Pierrot M, Mathonnet A, Béduneau G, Delétage-Métreau C, Richard JC, Brochard L, Robert R; FLORALI Study Group; REVA Network. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. 2015 Jun 4;372(23):2185-96. doi:10.1056/NEJMoa1503326. Epub 2015 May 17. PMID: 25981908.
[7] Renda T, Corrado A, Iskandar G, et al. High-flow nasal oxygen therapy in intensive care and anaesthesia. Br J Anaesth 2018; 120: 18–27.
[8] Luo JC, Lu MS, Zhao ZH, Jiang W, Xu B, Weng L, Li T, Du B. Positive End-Expiratory Pressure Effect of 3 High-Flow Nasal Cannula Devices. Respir Care. 2017 Jul;62(7):888-895. doi: 10.4187/respcare.05337. Epub 2017 Apr 25. PMID: 28442633.
[9] Möller W, Celik G, Feng S, Bartenstein P, Meyer G, Oliver E, Schmid O, Tatkov S. Nasal high flow clears anatomical dead space in upper airway models. J Appl Physiol (1985). 2015 Jun 15;118(12):1525-32. doi: 10.1152/japplphysiol.00934.2014. PMID: 25882385; PMCID: PMC4482836.
[10] Renda T, Corrado A, Iskandar G, et al. High-flow nasal oxygen therapy in intensive care and anaesthesia. Br J Anaesth 2018; 120: 18–27.
[11] ERS clinical practice guidelines: high-flow nasal cannula in acute respiratory failure. Simon Oczkowski, Begüm Ergan, Lieuwe Bos, Michelle Chatwin, Miguel Ferrer, Cesare Gregoretti, Leo Heunks, Jean-Pierre Frat, Federico Longhini, Stefano Nava, Paolo Navalesi, Aylin Ozsancak Uğurlu, Lara Pisani, Teresa Renda, Arnaud W. Thille, João Carlos Winck, Wolfram Windisch, Thomy Tonia, Jeanette Boyd, Giovanni Sotgiu, Raffaele Scale. European Respiratory Journal Apr 2022, 59 (4) 2101574; DOI: 10.1183/13993003.01574-2021
[12] Mussa CC, Gomaa D, Rowley DD, Schmidt U, Ginier E, Strickland SL. AARC Clinical Practice Guideline: Management of Adult Patients with Tracheostomy in the Acute Care Setting. Respir Care. 2021 Jan;66(1):156-169. doi: 10.4187/respcare.08206. Epub 2020 Sep 22. PMID: 32962998.
[13] Munshi L, Mancebo J, Brochard LJ. Noninvasive Respiratory Support for Adults with Acute Respiratory Failure. N Engl J Med. 2022 Nov 3;387(18):1688-1698. doi: 10.1056/NEJMra2204556. PMID: 36322846.
[14] Williams R, Rankin N, Smith T, Galler D, Seakins P. Relationship between the humidity and temperature of inspired gas and the function of the airway mucosa. Critical Care Medicine 1996; 24: 1920–9.
[15] Woods BD, Sladen RN. Perioperative considerations for the patient with asthma and bronchospasm. Br J Anaesth. 2009 Dec;103 Suppl 1: i57-65. doi: 10.1093/bja/aep271. PMID: 20007991. Perioperative considerations for the patient with asthma and bronchospasm – British Journal of Anaesthesia (bjanaesthesia.org)
[16] Fontanari P, Burnet H, Zattara-Hartmann MC, et al. Changes in airway resistance induced by nasal inhalation of cold dry, dry, or moist air in normal individuals. J Appl Physiol 1996;81(4): 1739e43. 27.
[17] Fontanari P, Zattara-Hartmann MC, Burnet H, et al. Nasal eupnoeic inhalation of cold, dry air increases airway resistance in asthmatic patients. Eur Respir J 1997;10(10):2250e4.
[18] Kevin Dysart, Thomas L. Miller, Marla R. Wolfson, Thomas H. Shaffer, Research in high flow therapy: Mechanisms of action, Respiratory Medicine, Volume 103, Issue 10, 2009, Pages 1400-1405, ISSN 0954-6111, https://doi.org/10.1016/j.rmed.2009.04.007.
[19] Möller W, Celik G, Feng S, Bartenstein P, Meyer G, Oliver E, Schmid O, Tatkov S. Nasal high flow clears anatomical dead space in upper airway models. J Appl Physiol (1985). 2015 Jun 15;118(12):1525-32. doi: 10.1152/japplphysiol.00934.2014. PMID: 25882385; PMCID: PMC4482836.

Ultra-soft nasal cannula
The NeoFlow® cannula features materials that improve patient comfort and experience.

Antimicrobial Protection
All NeoFlow® circuits have BioCote® protection which helps reduce the risk of infection in NICU and Paediatric wards.

Open platform
Our NeoFlow® circuitry can be used with various types of gas flow driver and humidifier.
Frequently Asked Questions
What flow rates should I start HFOT at in my neonatal patient?
How long can we use these circuits for?
Our NeoFlow® circuits are 7-day single patient use.
Is the addition of BioCote® dangerous for my neonatal patient?
BioCote® is an ingredient that we add during the manufacturing process, this makes it integral to the structure of the product so it cannot become displaced or harm the baby in any way.
Set up Guide
nHFOT Products
References
[1] Franklin, Donna, et al. “Effect of Early High-Flow Nasal Oxygen vs Standard Oxygen Therapy on Length of Hospital Stay in Hospitalized Children With Acute Hypoxemic Respiratory Failure: The PARIS-2 Randomized Clinical Trial.” JAMA 329.3 (2023): 224-234.
[2] Richards-Belle, Alvin et al. “FIRST-line support for assistance in breathing in children (FIRST-ABC): a master protocol of two randomised trials to evaluate the non-inferiority of high-flow nasal cannula (HFNC) versus continuous positive airway pressure (CPAP) for non-invasive respiratory support in paediatric critical care.” BMJ open vol. 10,8 e038002. 4 Aug. 2020, doi:10.1136/bmjopen-2020-038002
Get in touch
We are committed to protecting and preserving the privacy of our visitors when visiting our site or communicating electronically with us.