On this page

Why Mask Fit Matters in Non-Invasive Ventilation
Non-invasive ventilation (NIV) and Continuous Positive Airway Pressure (CPAP) are only as effective as the interface delivering them. A poorly fitting mask can lead to air leaks, discomfort, pressure injury, and ultimately therapy failure. In contrast, selecting the correct size and applying the mask correctly from the outset can significantly improve patient tolerance, protect skin integrity, and support positive clinical outcomes.
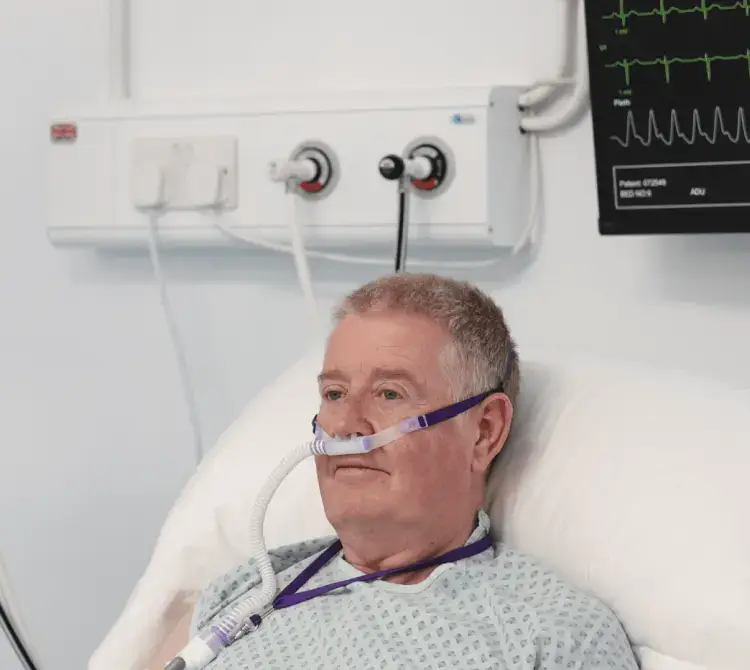
The V2 Oro-Nasal Mask has been designed to deliver effective ventilation while prioritising comfort, skin protection, and ease of use. Understanding how to size, fit, and adjust the mask allows clinicians to optimise therapy from the very first application.
Choosing the Right Mask Size: A Foundation for Success
Correct sizing is one of the most critical factors in achieving a reliable seal. The V2 Oro-Nasal Mask uses length-based facial measurements, enabling clinicians to select the most appropriate size quickly, accurately, and discreetly.
For accurate measurement, the patient’s facial muscles should be relaxed with the jaw closed. The sizing gauge is placed at the nasal bridge, just below the eyes, and the size is determined by where the bottom of the chin aligns with the gauge. If the measurement falls between two sizes, selecting the smaller size typically provides a more effective seal.
Individual facial anatomy should always be considered. Patients with beards, prominent soft tissue, or excess skin around the neck may require a larger size, while those with smaller facial features or no teeth may benefit from a smaller mask. With five sizes available, and Petite and Extra Small being the most used, the V2 mask range supports a precise, first-time fit for the majority of patients.
Applying the Mask: Comfort, Stability, and Alignment
Once the correct size has been selected, careful application helps ensure comfort, stability, and alignment.
The mask should be applied by gently rolling it from the chin upwards to cover the mouth and nose, allowing the seal to form naturally. This technique works alongside the integrated chin cup, which enhances stability and helps prevent upward movement into the patient’s line of sight.
Headgear should be positioned carefully, securing the top straps first, followed by the lower straps. Adjustments should be made while facing the patient, ensuring the mask follows the natural contours of the face. The straps should feel secure but not tight, there should be enough space to fit one finger between the strap and the skin.
The V2 mask is designed to minimise leaks without excessive tightening. Over- tightening can increase discomfort and significantly raise the risk of pressure injury, particularly over vulnerable areas such as the nasal bridge.
V2 NIV Facemasks
The V2 Mask range of adult oro-nasal masks from Hans Rudolph have low dead space, helping you deliver effective non-invasive ventilation and CPAP to your patient.
Managing Leaks Without Compromising Skin Integrity
Leak assessment is an essential part of mask optimisation. Asking the patient to exhale deeply allows clinicians to identify air escape around the nose, cheeks, or chin.
Minor leaks can often be corrected by adjusting the strap at the crown of the head, rather than tightening all straps. This approach helps maintain comfort while preserving the integrity of the seal.
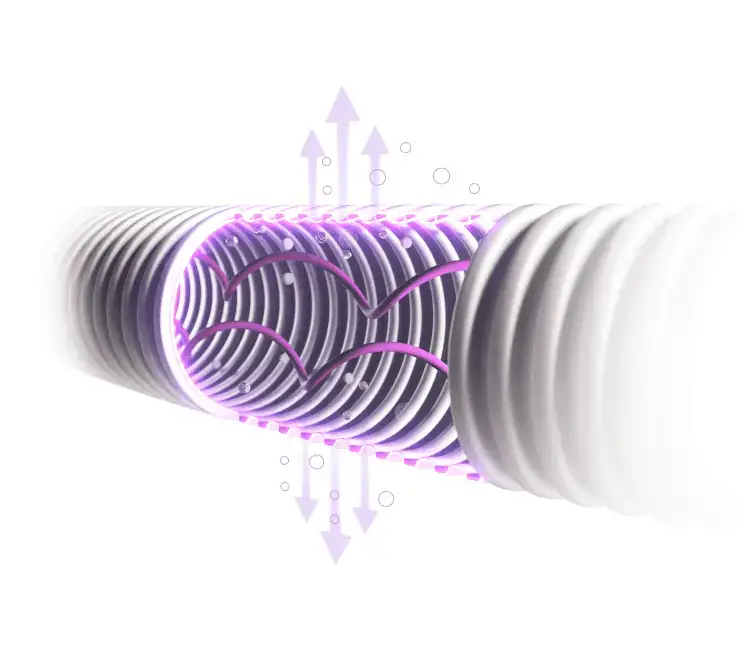
A key feature of the V2 mask is its deep, dual-seal nasal flange, manufactured from soft thermoplastic elastomer. This design creates a low-pressure seal at the nasal bridge, reducing leaks while minimising pressure on the skin. Excessive tightening can impair this mechanism and increase the risk of skin damage.
Protecting the Skin During NIV Therapy
Device-related pressure injuries (DRPIs) occur when medical devices exert sustained mechanical load on the skin and underlying tissues. These injuries typically conform to the shape of the device and are most likely to occur at the device–skin interface, where pressure, shear, and friction are concentrated.
International pressure injury prevention guidelines 2025[1] emphasise the importance of:
- Selecting medical devices with appropriate design, construction materials, and sizing
- Ensuring devices conform to individual anatomy
- Reassessing fit regularly, particularly in patients experiencing fluid shifts, oedema, or weight change
- Avoiding rigid materials over pressure-prone areas
- Following manufacturer guidance and avoiding off-label use
Regular skin assessments should be performed on admission and at least every four hours during NIV therapy[2], with particular attention to the nasal bridge and chin. Assessment frequency should increase for individuals at higher risk, including those with fragile skin, diaphoresis, reduced sensation, or limited ability to communicate discomfort.
If early signs of skin compromise are observed, such as blanchable or non-blanchable erythema, a thin preventive foam dressing may be applied to help redistribute pressure[2], provided it does not interfere with mask fit or function. Dressings should allow adequate heat and moisture transfer to avoid maceration, and care should be taken to ensure that additional layers do not increase pressure under tightly fitted devices[1].
The V2 mask’s anatomically contoured design and absence of rigid components over high-risk areas further support skin protection when used as intended.
Understanding Why Mask-Related Injuries Occur
Pressure injuries are localised damage to the skin and underlying tissue, typically over bony prominences or beneath medical devices, resulting from prolonged pressure or pressure combined with shear. Injury can occur beneath intact skin or present as an open ulcer and may be painful.[1]
In the context of NIV, mask-related injuries rarely occur due to pressure alone. Instead, they result from a combination of:
- Pressure - restricting blood flow
- Shear - distorting tissues and blood vessels
- Friction - causing superficial skin damage
- Microclimate changes - including heat and moisture buildup under the mask
Together, these factors compromise tissue tolerance and increase the risk of injury, particularly over vulnerable facial anatomy such as the nasal bridge[1].
Supporting Patient Comfort and Ongoing Care
Patient comfort is central to NIV tolerance and success. Where clinically appropriate, intermittent breaks using nasal cannula or high-flow oxygen can help maintain comfort and allow time for essential care such as oral hygiene, medication administration, and skin inspection[3,4].
It is considered good practice to reduce or redistribute pressure by alternating oxygen delivery interfaces when safe to do so, and by regularly repositioning the device and its securements to minimise pressure and shear forces[1].
For patients requiring nasogastric tubes, applying a MetroSeal™ NG securement device prior to mask fitting can help reduce leaks and improve comfort by creating a more effective seal around the tube.
Mask removal is straightforward, using the quick-release clasps on the lower straps before gently lifting the mask away from the chin and nose.
Designed for Flexibility Across Clinical Settings
The V2 Oro-Nasal Mask range includes vented and non-vented configurations, supporting use across a wide range of ventilation systems.
Non-vented masks are intended for use with mechanical ventilators in acute care settings, relying on ventilator safety systems. Options incorporating an anti-asphyxia valve provide an additional layer of safety, allowing room air entrainment in the event of ventilator failure or power loss. Vented versions are designed for single-limb bi-level devices, ensuring effective exhalation while maintaining patient safety.
This versatility reduces the need to stock multiple mask types, simplifying inventory management while maintaining clinical safety.
A Thoughtful Interface for Effective NIV
The V2 Oro-Nasal Mask combines low dead space, anatomical design, and evidence-informed features to support effective ventilation, CO₂ clearance, and patient comfort. When paired with correct sizing, careful application, and regular reassessment, it enables clinicians to deliver NIV that is both effective and well-tolerated.
By focusing on fit, comfort, and skin protection, clinicians can reduce complications, improve patient experience, and support better therapy outcomes.

Abby Lennon
Clinical Nurse Adviser, RN
Abby works alongside the Clinical Education Team to provide support and education to healthcare professionals using her knowledge and experience as a registered nurse working in respiratory wards and intensive care units over the last eight years.
References
[1] National Pressure Injury Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. Device-Related Pressure Injuries. In: Prevention and Treatment of Pressure Ulcers/Injuries: Clinical Practice Guideline. The International Guideline: Fourth Edition. Emily Haesler (Ed.). 2025.Available from: https://internationalguideline.com.
[2] Gefen, Amit, et al. “Device-Related Pressure Ulcers: SECURE Prevention. Second Edition.” Journal of Wound Care, vol. 31, no. Sup3a, 1 Mar. 2022, pp. S1–S72, https://doi.org/10.12968/jowc.2022.31.sup3a.s1.
[3] Davidson, A Craig, et al. “BTS/ICS Guideline for the Ventilatory Management of Acute Hypercapnic Respiratory Failure in Adults.” Thorax, vol. 71, no. Suppl 2, 14 Mar. 2016, pp. ii1–ii35, https://doi.org/10.1136/thoraxjnl-2015-208209.
[4] Amir Emami Zeydi, et al. “Mask‐Related Pressure Injury Prevention Associated with Non‐Invasive Ventilation: A Systematic Review.” International Wound Journal, vol. 21, no. 6, 1 June 2024, https://doi.org/10.1111/iwj.14909.