The benefits of heated, humidified gases in the delivery suite
- Published on:
The benefits of heated, humidified gases in the delivery suite
- Published on:

On this page

Introduction
The care of babies, born early or sick, has changed massively in the last 40 years, with positive advances in properly researched methods of treatment and improved medical device technologies, helping to carve out a standalone role for healthcare professionals who previously would have looked after ‘paediatrics’ as a generic speciality. Doctors and nurses now practicing in the field of ‘neonatology’ have experienced a significant shift, as the size of their patients has got progressively smaller, while the expected outcomes for these babies have continuously improved. Many simple, and other novel techniques and therapies have been introduced and implemented over the years that mean we now care for babies smaller and more fragile than ever before.
The sight of premature babies being cared for in tiny glass cabinets, such as those being looked after by Dr Martin Couney’s nurses on Coney Island, New York, USA is somewhat of a distant memory with specialised equipment such as servo-controlled incubators now protecting these tiny babies and providing a warm environment in which they can grow and develop.
Thermoregulation
Thermoregulation This increasingly complex group of extremely preterm infants come with their own set of challenges, not least the difficulty of keeping warm. Thermoregulation and prevention of hypothermia is already high on the list of priorities in maternity departments delivering healthy term babies. However, in the same environment where the Very Low Birth Weight (VLBW) infant is exceedingly more fragile and affected by heat loss, other techniques may need to be adopted to prevent dangerous decreases in core body temperature. International recommendations require the core body temperature of a newborn be kept within a range of 36.5°C – 37.5°C to provide the best outcomes for that baby[1] and neonatal units record the temperature of babies upon admission as a marker of quality of care and predicted patient outcome. Studies have shown that even as little as a 1°C drop in admission temperature increases the risk of sepsis in a VLBW newborn by 11% with the overall risk of morbidity increasing by 28%[2][3].
Couple these statistics with the evidence that body temperature can fall by as much as 4°C in the first 10-20 minutes of life, if the newborn infant is left without thermal protection[4], the risk and associated outcomes of hypothermia to VLBW infants are profound. Given this evidence base, perinatal teams put extensive efforts in to ensuring that babies admitted to neonatal care have admission temperatures recorded within the normal range. Various pieces of equipment are available that may provide a positive impact immediately post-delivery, and before baby is admitted to the neonatal unit[2].
These include a specially designed polythene bag or suit that acts like a ‘greenhouse’ around a newly delivered infant to trap heat inside (Image1) and standalone combination warmers and resuscitation units that provide a prewarmed surface with a radiant heat source and respiratory support device built in, that provides a warmed environment and external heat source to a baby as medical staff complete relevant checks and provide respiratory support if needed (Image 2).

(Image 2 – GE Giraffe Warmer) Giraffe
Warmer | GE Healthcare (United States)
(Image 1- Vygon Neohelp™) Vygon
Neohelp Heat Loss Bag – Medsales
Both or either of these options may already be well implemented in practice within most maternity and neonatal departments but an additional complementary option is available that may have a significant impact on thermoregulation and provide a very positive outcome when used in conjunction with current practice.
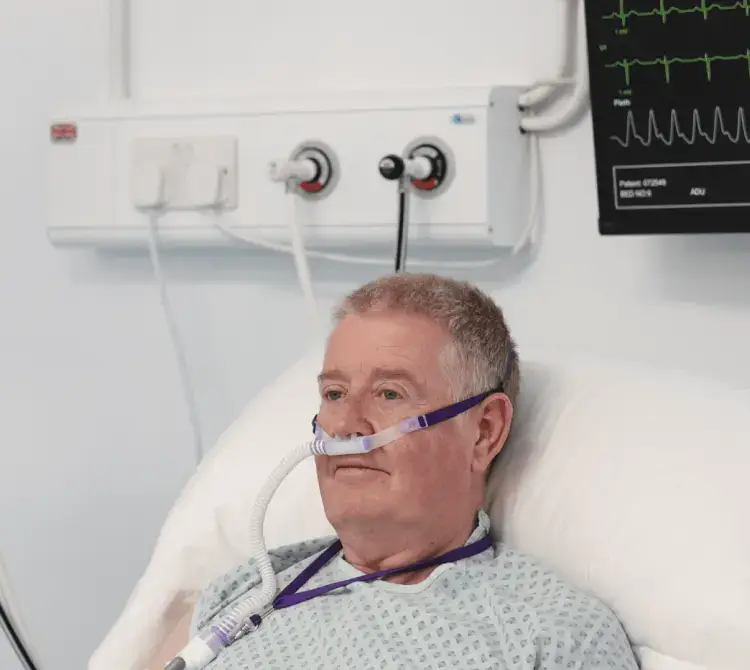
Stabilisation
Meyer et al.[5], have shown the benefits of using warmed gases when stabilising VLBW infants and providing Positive Pressure Ventilation (PPV) or respiratory stabilisation. The VLBW infant that may especially benefit from the polythene bag or radiant warmer is also much more likely to require respiratory support or be offered respiratory support immediately after birth compared to a term baby [6]. Current practice in many countries see babies requiring this respiratory support provided a platform bed, (e.g, Image 2 above) and via a t-piece resuscitation device built into the upright manifold extending from the back of the bed. This allows for the oxygen rich gases and positive pressure to be initiated almost instantly for the 10% of babies that do not breathe when they are born[7].
However, the gases delivered through this PPV system come directly from a piped gas source or gas cylinders and as a result can be described as ‘cold and dry’. In fact, an investigation carried out across different areas in one hospital demonstrated piped oxygen having a mean temperature of 23.3°C and a Relative Humidity (RH) of only 2.1%, while piped air was measured at 23.4°C with a RH of 5.4%[8], rather stark findings. With the already fragile VLBW baby receiving PPV and stabilisation with these cold and dry gases it follows a simple train of thought that this could lead to the infant’s body temperature lowering outside of the recommended range.
At the very least we can expect that given the massive impact of conduction, convection, radiation, and evaporation [9] on these premature babies, the cold and dry gases are not useful in combating the heat loss associated with these thermodynamic forces, and that the use of warmed and humidified gases, as suggested in the 2014 study by Meyer et al.[5], would assist with this.
A further meta-analysis of additional studies using heated, humidified resuscitation to stabilise babies needing respiratory support at birth included a total of 476 preterm infants <32 weeks gestation. The analysis showed a reduction in admission hypothermia by 36% in the heated, humidified group supporting their recommendation to consider heating and humidification of inspired gases during stabilisation after birth and during transport to the neonatal unit [10].
Heated Humidified Gas
The concept of humidified gases in the neonatal environment is not alien, after all, it is widely accepted and practiced that any therapeutic and supportive acute respiratory therapies delivered in the neonatal ward setting are done so with active heat and humidification. A heated wire limb and humidification chamber are familiar items in the Neonatal Intensive Care Unit (NICU) and can be included in a pack to create a heated, humidified t-piece circuit that will deliver pressures and PPV breaths in the same format as a standard non-heated alternative. The heated wire limb and humidification chamber both work in conjunction with an electrical heater humidifier supplying a heat source and heater wire power to add heat and water vapour to the system as gas passes through the humidification chamber. With this type of system already a familiar sight in NICUs globally it should not require extensive additional training to operate.
References
Wyckoff, Myra H., et al. “Neonatal life support: 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations.” Circulation 142.16_suppl_1 (2020): S185-S221.
2. McCall, Emma M., et al. “Interventions to prevent hypothermia at birth in preterm and/or low birth weight infants.” Cochrane Database of Systematic Reviews 2 (2018).
3. Laptook, Abbot R., et al. “Admission temperature of low birth weight infants: predictors and associated morbidities.” Pediatrics 119.3 (2007): e643-e649.
4. World Health Organization. Thermal protection of the newborn: a practical guide. No. WHO/RHT/MSM/97.2. World Health Organization, 1997.
5. Meyer, Michael P., et al. “Initial respiratory support with cold, dry gas versus heated humidified gas and admission temperature of preterm infants.” The Journal of Pediatrics 166.2 (2015): 245-250.
6. Newborn resuscitation and support of transition of infants at birth Guidelines | Resuscitation Council UK
7. Madar, John, et al. “European Resuscitation Council Guidelines 2021: Newborn resuscitation and support of transition of infants at birth.” Resuscitation 161 (2021): 291-326.
8. Dawson, Jennifer A., et al. “Quantifying temperature and relative humidity of medical gases used for newborn resuscitation.” Journal of Paediatrics and Child Health 50.1 (2014): 24-26.
9. Knobel, Robin, and Diane Holditch‐Davis. “Thermoregulation and heat loss prevention after birth and during neonatal intensive‐care unit stabilization of extremely low‐birthweight infants.” Journal of Obstetric, Gynecologic & Neonatal Nursing 36.3 (2007): 280-287.
10. Meyer, Michael P., Louise S. Owen, and Arjan B. Te Pas. “Use of heated humidified gases for early stabilization of preterm infants: a meta-analysis.” Frontiers in Pediatrics 6 (2018): 319.
11. Bustamante-Marin, Ximena M., and Lawrence E. Ostrowski. “Cilia and mucociliary clearance.” Cold Spring Harbor perspectives in biology 9.4 (2017): a028241.
Download Clinical Paper