Home > Stabilisation
Stabilisation
Stabilisation
What is Stabilisation?
Stabilisation establishes or assists with effective ventilation in the crucial first few minutes of life for around 10% of babies who require assistance to start breathing and adapt to life outside the womb [1]. This can be done using a standard T-piece resuscitation circuit but can also be provided using heated gas during delivery-room stabilisation, this has also been observed to reduce the rate of moderate hypothermia on admission to the NICU, with no increased risk of hypothermia [2].

Supports Cardiovascular Transition
as the baby’s circulation must shift from placental to independent oxygenation. This transition is vital to maintaining stable heart rate and blood pressure [4].
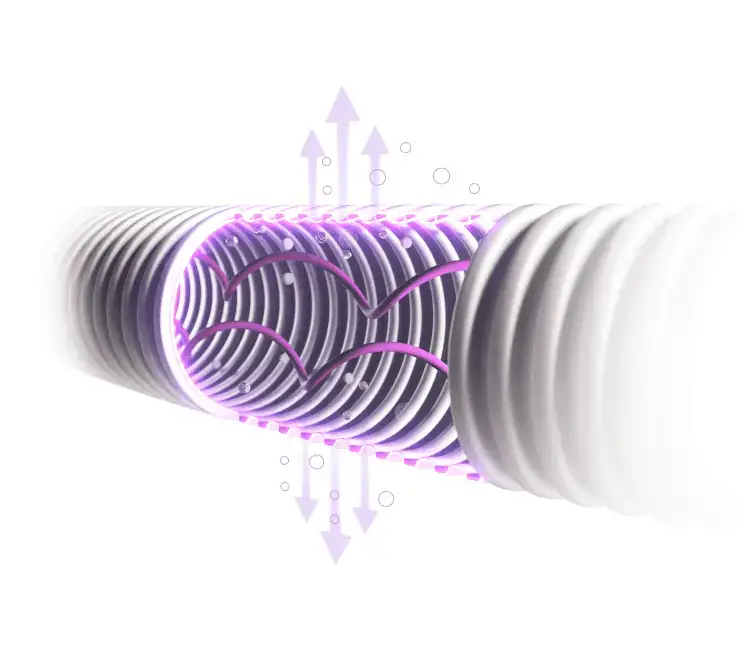
The use of humidified gases has been shown to provide improvements in admission temperature (i.e., a reduction in instance of hypothermia) [7,8] while also supporting better respiratory function[9]. NeoFlow® humidified resuscitation limbs can provide respiratory support through both face mask or tracheal tube and can be transitioned to provide Delivery Room CPAP.

Improved Thermal Stability

Enhanced Respiratory Performance

Face Masks or Nasal Interface Compatibility
Provides delivery of warm, humidified gas via face masks or nasal interfaces, helping to maintain neonatal body temperature and airway humidity for improved respiratory support.
Frequently Asked Questions
Will the NeoFlow® Heated Resuscitation Circuit work with my existing set up?
Accommodates all types of neonatal resuscitation devices with additional connectors provided if required.
Why should I use NeoFlow® Heated Resuscitation circuits?
NeoFlow® Circuits are BioCote protected, providing antimicrobial protection while circuit is set up in anticipation for babies requiring support.
Video Material
Our NeoFlow® resuscitation limbs can support through a face mask or tracheal tube with the intention of providing positive end-expiratory pressure (PEEP) and positive inspiratory pressure (PIP) via adjustment of a pressure control cap.
BioCote® Protected
Our NeoFlow® Circuits are BioCote® protected, providing antimicrobial protection while circuit is set up in anticipation for babies requiring support.

Accurate Pressure Delivery
Easy to use, tactile PIP control cap with linear and proportional adjustment of pressure.

Resus Face Mask
Available in 4 sizes, designed to provide a secure seal with minimum pressure on sensitive skin.
- Satin sealing surface
- Feather thin edge
- Non-collapse crown
- Hand positioning guide for optimal seal and ventilation
- Finger grooves
Frequently Asked Questions
I have multiple different machine across my hospital, how does the NeoFlow® product help me?
NeoFlow® T-Piece resuscitation circuits can be configured with your desired connector combination to ensure that one kit is compatible with the various different machine types in your hospital.
Can these circuits be used while we deliver delayed cord clamping?
Yes. NeoFlow® T-Piece resuscitation circuits are available in long and extra long lengths to assist with the stabilisation of baby while performing delayed cord clamping (DCC). This means you can use equipment already at hand and not have to purchase DCC specific trollies or platforms.
Is the addition of BioCote® dangerous for my neonatal patient?
No. BioCote® is an ingredient added during the manufacturing process, making it integral to the product structure. It cannot become displaced or harm the baby in any way, BioCote® provides antimicrobial protection to the build to prevent microbe colonisation.
NeoFlow® Neonatal Resuscitation
Delivery Room CPAP or DR CPAP is the use of Continuous Positive Airway Pressure therapy immediately after birth in the delivery suite or labour ward. This positive pressure helps with alveolar recruitment and forming the functional residual capacity, supporting a baby who must transition from fluid filled lungs in the womb to air filled lungs after delivery.

Early CPAP Usage
Early CPAP usage in neonates has been found to have the ability to reduce the need for a baby to be intubated.

Respiratory Support on the Cord
Extra long length allows PEEP.

Backed by Evidence
Studies have shown that allowing the baby to aerate their lungs before the cord is clamped, which may require some PEEP support, allows for a more physiologically stable transition after birth.
Frequently Asked Questions
Can I use the NeoFlow® circuit to Delivery Room CPAP as well as conventional resuscitation via a facemask?
NeoFlow® circuits facilitate easy transition from nasal CPAP delivery to face mask resuscitation if needed.
How can I introduce CPAP in the Delivery Suite?
The introduction of a CPAP system in the delivery suite is dependent on the equipment already in use, but is often very simple and straightforward to implement.
The specialised NeoFlow® delivery room CPAP circuit along with CPAP interface and hat can work along side any standard resuscitator to provide delivery room CPAP via the nasal interface, requiring no specialized CPAP machines, which helps keeps cost lower. For humidified delivery room CPAP, a heater humidifier can be added to the side of the radiant warmer, or mounted to the resuscitator on a receiving platform or trolley, using a heated circuit option you can delivery warm humidifed therapy to baby.
Supporting Newborns from their First Breath
Stabilisation Products
References
[3] Perlman JM, Wyllie J, Kattwinkel J, et al. Part 7: Neonatal Resuscitation: 2015 International Consensus on CPR and ECC Science With Treatment Recommendations. Resuscitation. 2015;95:e169–e201.
[4] Hooper SB, Te Pas AB, Kitchen MJ. Respiratory transition in the newborn: a three-phase process. Arch Dis Child Fetal Neonatal Ed. 2016;101(3):F266–F271. doi:10.1136/archdischild-2013-305704.
[5] European Resuscitation Council Guidelines 2025 Newborn Resuscitation and Support of Transition of Infants at Birth. Resuscitation 2025;215 (Suppl 1):110766. https://doi.org/10.1016/j.resuscitation.2025.110766
[8] Meyer MP, Te Pas AB, Owen LS, et al. Initial respiratory support with cold, dry gas versus heated humidified gas and admission temperature of preterm infants. Journal of Pediatrics (or the actual journal). 2015;[volume(issue)]:[pages]. doi:10.1016/j.jpeds.2014.09.007
[9] McGrory L, Shah PS, Lee SK, et al. A randomized trial of conditioned or unconditioned gases for stabilizing preterm infants at birth. Journal of Pediatrics. 2018;[volume(issue)]:[pages]. doi:10.1016/S0022-3476(17)31167-8
Get in touch
We are committed to protecting and preserving the privacy of our visitors when visiting our site or communicating electronically with us.