The benefits of heating and humidifying gases in the perioperative setting
- Published on:
The benefits of heating and humidifying gases in the perioperative setting
- Published on:


The use of heated and humidified gases in the perioperative setting has become increasingly popular in recent years due to its numerous benefits for both the patient and the surgical team. This month’s blog will discuss the importance of using heated and humidified gases, the various devices available for providing this, and the evidence supporting their use in the perioperative setting.
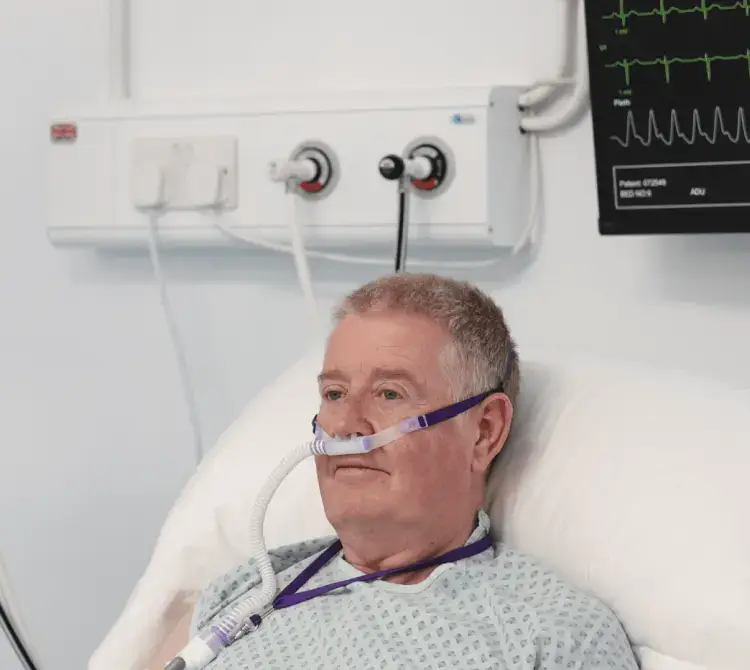
These gases are typically oxygen, air, or nitrous oxide, and can be heated and humidified before being delivered to the patient through a breathing circuit or mask. This practice, known as peri-operative humidification, is typically used to reduce the risk of complications and improve patient comfort during surgery.
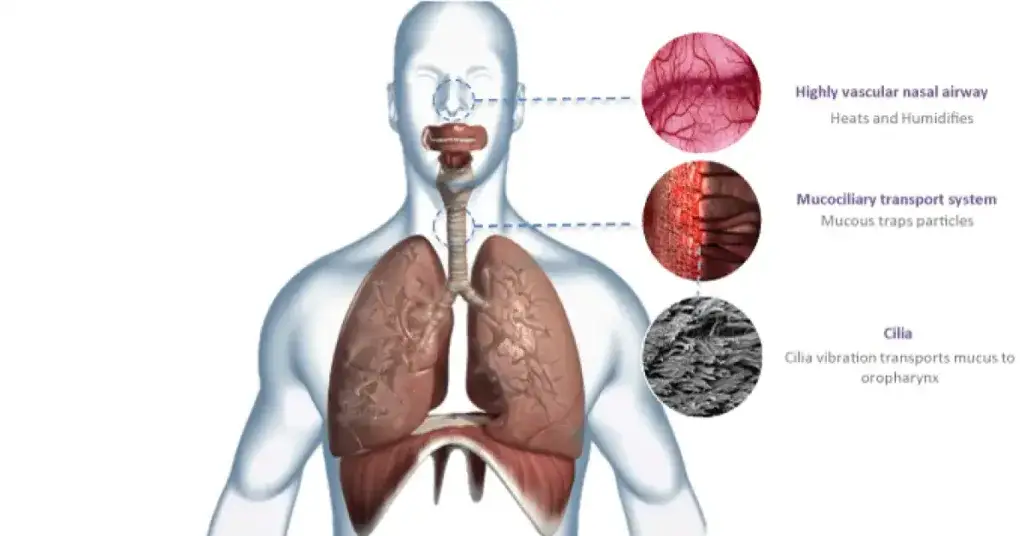
During surgery, the airway can become dry due to a variety of factors, including the use of anaesthesia, the administration of dry oxygen through a breathing circuit, and the natural evaporation of moisture from the airway [1]. When a patient’s trachea is intubated or a supraglottic airway device is placed in situ, the normal warming, humidifying, and filtering functions of the upper airways are bypassed. With inadequate humidity being delivered directly to the trachea; damage can occur to the lining of the trachea [1].
This dryness can cause the airway to become inflamed, which can lead to complications such as coughing, laryngeal spasm, and bronchoconstriction [2]. The patient is already at an increased risk of airway obstruction as the decrease in muscle tone associated with loss of wakefulness is compounded by specific drug‐induced inhibition of upper airway neural and muscle activity. Although the incidence of severe perioperative bronchospasm is low, in high-risk patients undergoing anaesthesia, when it does occur it can be life threatening due to obstruction of the airway [4]. Furthermore, Fontanari and colleagues showed that receptors in the nasal mucosa respond to cold and dry gas to elicit a protective bronchoconstrictor response in both normal subjects and asthmatics [5,6]
Chalon and colleagues showed that after less than 4 hours of mechanical ventilation, anesthetised patients who received inadequately humidified gas had significantly more postoperative complications than patients who received saturated gas [7]. By providing moist, warm gases to the airway, peri-operative humidification helps keep the airway hydrated and reduces the risk of these complications.
Mucociliary clearance, effected by the coordinated beating of cilia, is the first line of defence to maintain pulmonary health and is responsible for clearing both the upper (nasal cavity) and lower airways of mucus, particulate matter, and pathogens. Williams et al. described a range of dysfunction that can occur in the respiratory tract if the humidity and temperature of the delivered gas to a patient are not optimal [8]. These include thickened mucus, causing mucociliary transport to slow or stop, reduced ciliary movement, causing cell damage and decreased lung compliance, and reducing functional residual capacity which can lead to atelectasis and shunting [8]. A study by Hansani et al, showed that warm air humidification treatment improved lung mucociliary clearance in bronchiectasis patients [9]. Hence, gas delivered to the patient needs to be artificially conditioned to replace these lost functions.
There are several studies that discuss the benefits of using heated and humidified gases with nasal high flow oxygen pre and peri-operatively, including rapid sequence induction [10,11]. The purpose of this being to extend the apnoeic window before the airway is secured. High flow oxygen with heated and humidified gases was shown to be non-inferior to oxygen delivered face mask and has been shown to reduce the increase in arterial carbon dioxide levels during apnoea by 50% [10]
When the patient receives a warm and moist gas mixture before the surgery, it can reduce the risk of postoperative complications [11]. After a surgical procedure, the patient may experience irritation and inflammation in their airways, leading to coughing, difficulty breathing, and other respiratory problems. Heating and humidifying the gas can ensure patient comfort, alleviate patient anxiety, and help reduce the need for additional pain medications, which can have side effects such as drowsiness and nausea [12].
Furthermore, in theatre general anaesthesia and inadvertent hypothermia is by far the most common perioperative thermal disturbance; it results from a combination of anaesthetic-impaired thermoregulation and exposure to a cold operating room environment [13]. This along with the exposure of body cavities and blood loss can trigger autonomic defences and lead to hypothermia, which is associated with increased morbidity and mortality in surgical patients [14].
Perioperative hypothermia is defined as a core temperature of below 36°C and is a common adverse consequence of anaesthesia and surgery. Hypothermia in most patients undergoing general anaesthesia is the result of an internal core-to-peripheral redistribution of body heat that usually reduces core temperature by 0.5– 1.5°C in the first 30 min after induction [12].
Several meta-analyses and RCTs (Randomised Controlled Trials) have demonstrated that preventing inadvertent hypothermia during major abdominal surgery significantly reduces wound infections [14], cardiac complications, bleeding, and transfusion requirements, whilst improving the immune function, the duration of post-anaesthetic recovery and overall survival [15,16]. Therefore, it makes sense to prevent the loss of body heat as recommended by the ERAS (Enhanced Recovery After Surgery) society. Combined strategies including heated and humidified gases, should be considered in vulnerable groups such as older patients with cardiorespiratory diseases, and surgery of long duration [12].
The heated gases can help maintain normothermia by providing a warm and moist environment for the patient. The gases are heated to a temperature of 37-38°C, which is normal body temperature. The gases are humidified to a relative humidity of 100%, which helps prevent dehydration of the mucous membranes, therefore maintaining normothermia by reducing heat loss through the respiratory tract [17].
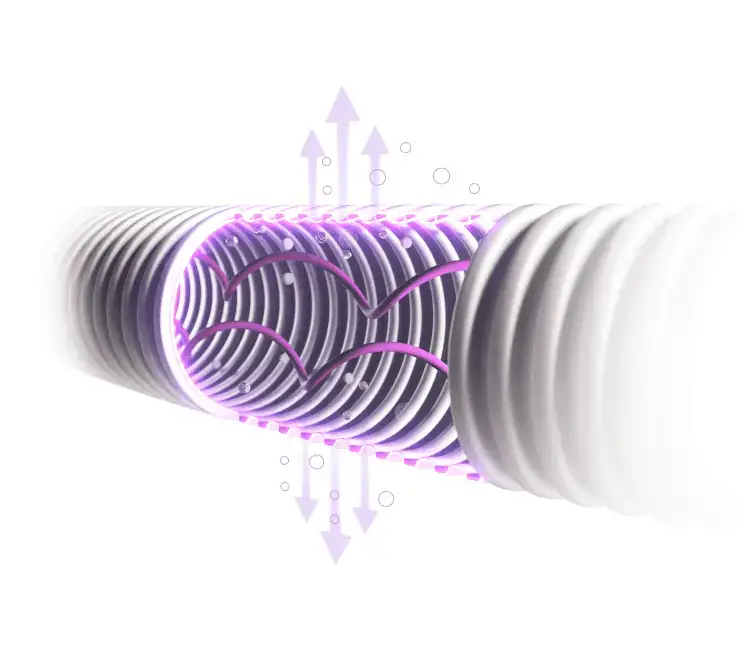
There are several types of devices available that provide heated and humidified gases in the perioperative period. One common type of device is a heater humidifier, which heats and humidifies the gases as they pass through a water chamber [18]. Another method is to use a heat and moisture exchanger, which is a device placed between the patient and the breathing circuit or mask. The exchanger captures the moisture from the patient’s exhaled breath and uses it to humidify and warm the gases that are delivered to the patient [19].
Despite the clear benefits of using heated and humidified gases in the operating theatre, there are also some challenges and considerations that need to be considered. One of the main challenges is the cost. Heating and humidifying gases requires additional equipment and trained personnel and can add to the overall cost of surgery.
Another challenge is the potential for increased risk of infection. Humidifying gases can create a more hospitable environment for bacteria and other pathogens, which can potentially increase the risk of infection to patients and healthcare workers. This risk can be mitigated through infection control measures, such as regular cleaning and maintenance of the humidification equipment, and by using sterile water and filters in the humidification process [20].
The evidence supporting the use of heated and humidified gases in the perioperative period is strong, as several studies have demonstrated. The benefits include improved patient comfort, improved surgical visibility, and reduced risk of complications [18,19].
In conclusion, the use of heated and humidified gases in the perioperative period has numerous benefits for both the patient and the surgical team as discussed above. Given the compelling evidence supporting their use, it is therefore important for surgical teams to consider the use of these gases in the perioperative period.