Intraventricular Haemorrhage in Preterm Infants: Pathophysiology, Risk Factors, and Management
- Published on:
Intraventricular Haemorrhage in Preterm Infants: Pathophysiology, Risk Factors, and Management
- Published on:

On this page

Intraventricular haemorrhage (IVH) is a critical complication in preterm infants, predominantly affecting those born before 30 weeks of gestation or weighing less than 1500 grams. Although improvements in perinatal and neonatal care have increased the survival rate of preterm infants, particularly those born at a gestational age of less than 25 weeks1, IVH continues to be a significant source of morbidity and mortality. The incidence of IVH in such infants remains approximately 25–30%2,3. These findings highlight the challenge of determining optimal management strategies for IVH. This review provides an overview of IVH pathophysiology, risk factors, and management, emphasising evidence-based approaches across antenatal, perinatal, and postnatal care.
Pathophysiology of IVH
IVH primarily originates in the germinal matrix, a transient, highly metabolically active, and highly perfused cell layer along the lateral ventricles. This layer is responsible for the precursors of cortical neurons and hemispheric glial cells, which subsequently migrate peripherally in a programmed pattern. The germinal matrix is most active during early gestation and progressively involutes, with only a small residual component remaining at the caudothalamic groove by 32–34 weeks of gestation4. The high vascularity of the germinal matrix makes it particularly vulnerable to haemorrhage, especially in preterm infants, where its immature vasculature—characterised by thin-walled capillaries—is prone to rupture under stress. Contributing factors to this vulnerability include:
- Immature Cerebral Autoregulation (CAR): Preterm infants lack robust autoregulatory mechanisms to stabilise cerebral blood flow (CBF), making the brain susceptible to injury from hypotension, hypertension, or fluctuations in systemic blood pressure5,6.
- Inflammatory and Hypoxic Factors: Conditions such as chorioamnionitis and postnatal sepsis exacerbate endothelial damage, increasing the risk of IVH. (7)
- Metabolic Instabilities: Hypoxia, hypercarbia, and acidosis destabilise the fragile vasculature of the germinal matrix8,9.
Risk Factors For IVH
Prenatal Risk Factors:
- Low Gestational Age and Birth Weight: The most important risk factor for germinal matrix IVH is very low gestational age. Infants born at <30 weeks gestation or weighing <1000 grams are at greatest risk.
- Chorioamnionitis and Maternal Infections: Maternal inflammation contributes to early cerebrovascular damage9.
Postnatal Risk Factors:
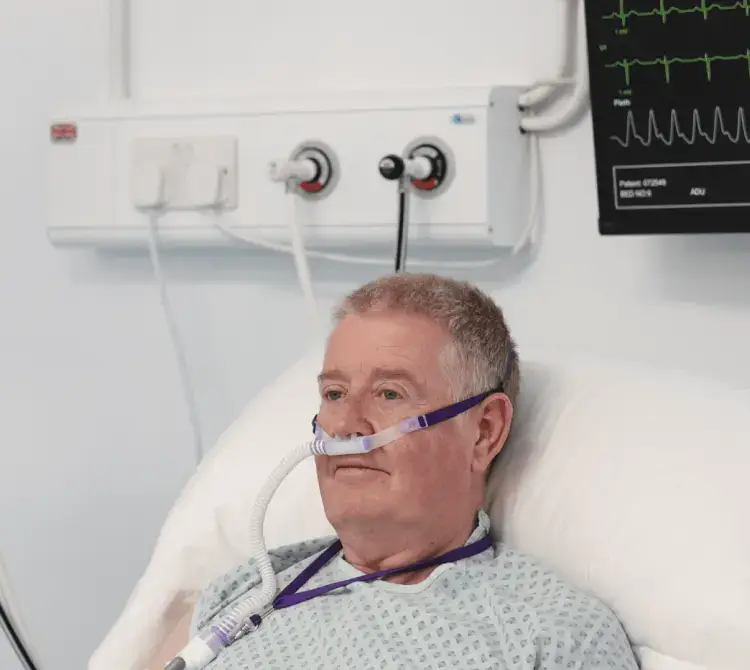
- Respiratory Distress Syndrome (RDS): Hypoxia and associated mechanical ventilation challenges increase IVH susceptibility.
- Fluctuations in Systemic Pressures: Hypotension or hypertension can lead to cerebral vessel rupture.
- Hypernatremia and Rapid Fluid Administration: These can disrupt osmotic gradients and exacerbate the risk of capillary leakage.
- Sepsis and Coagulopathy: Both amplify inflammatory cascades and endothelial injury.
Diagnosis and Grading
Ultrasonography: Cranial ultrasonography is the gold standard for IVH diagnosis, allowing early detection of bleeding and monitoring for complications like post-haemorrhagic ventricular dilatation (PHVD).
Papile Grading System8:
- Grade I: Haemorrhage confined to the germinal matrix.
- Grade II: Haemorrhage extending into the ventricles but without dilation.
- Grade III: Ventricular haemorrhage with accompanying dilation.
- Grade IV: Parenchymal extension, also termed periventricular haemorrhagic infarction (PVHI).
MRI for Prognosis: While cranial ultrasonography remains the gold standard for routine monitoring and early detection of IVH, it has limitations, particularly in detecting minor injuries to the cerebellum and grey and white matter. Magnetic resonance imaging (MRI) is considered superior for visualizing white matter injury and providing a more comprehensive assessment of brain damage. However, MRI poses several challenges for widespread use in preterm infants. It is difficult to perform in the early period because most neonates are unstable for transportation, the imaging process is time-consuming, anaesthesia is required, and it is an expensive procedure. Additionally, it may not alter management in the early stages. Despite these challenges, studies have shown that MRI, particularly for assessing white matter injury, is more effective when performed after the postconceptional age of 40 weeks. At this stage, MRI can offer valuable insights into both short- and long-term neurodevelopmental outcomes.
Prevention and Management
Antenatal Management:
- Antenatal Corticosteroids: Proven to reduce IVH incidence by stabilising the immature cerebrovascular architecture and improving neonatal respiratory outcomes. Studies show that administering corticosteroids 24 hours to 7 days before preterm birth significantly reduces the incidence of severe IVH in infants born at 22–29 weeks gestation. Antenatal steroids are also associated with improved RDS and reduced duration of mechanical ventilation10,11,12.
- Magnesium Sulphate: Administered during preterm labour, it decreases the risk of cerebral palsy (CP) in surviving neonates, although its direct effect on IVH prevention is less clear.
- Maternal Transfer to Specialised Centres with Neonatal Intensive Care Units: Facilities with neonatal intensive care units (NICUs) improve survival rates and reduce severe IVH through advanced resources and protocols.
Perinatal Management:
- Delayed Cord Clamping (DCC): DCC performed for 30–60 seconds post-delivery improves circulatory stability by increasing blood volume and haemoglobin levels. Evidence shows that DCC reduces the risk of severe IVH by up to 50%13.
- Optimising Delivery Room Practices: Ensuring thermal stability, gentle handling, and minimising large hemodynamic changes are crucial in reducing IVH risk immediately after birth.
Postnatal Management:
- Ventilation Strategies: Volume-targeted ventilation (VTV) reduces IVH risk by minimising large tidal volume fluctuations. VTV has been shown to reduce the incidence of severe IVH and chronic lung disease compared to pressure-limited ventilation14.
- Carbon Dioxide (CO2) Management: Tight CO2 control is critical, as both hypercapnia and hypocapnia increase IVH risk due to rapid cerebrovascular changes15,16.
- Prevention of Blood Pressure Extremes: Maintaining optimal blood pressure is critical in preterm infants, as both hypotension and hypertension are associated with an increased risk of IVH. Hypotension affects 15–50% of extremely preterm infants, although no universally accepted definition of normal blood pressure exists for this population. A common practice among neonatologists is to define hypotension as a mean arterial blood pressure (ABP) lower than the infant's gestational age in weeks. However, blood pressure alone is not a reliable indicator of cerebral or systemic perfusion. Administering inotropic drugs or volume expansion to hypotensive preterm infants who display clinical signs of adequate perfusion may be unnecessary and could inadvertently increase the risk of IVH17.
Neonatal Bundle of Care for IVH Prevention:
Optimising the care of preterm infants during the critical first 72 hours of life has been extensively studied as a strategy to reduce the incidence of IVH. However, results across studies remain inconsistent, highlighting the need for further research to establish optimal management protocols. Commonly accepted practices include18,19,20,21.
- Maintaining a supine midline position with the head in a neutral orientation.
- Tilting the incubator at a 10°C to 30°C incline to avoid the head-down position.
- Minimising handling, including limiting suction.
- Avoiding rapid flushes or blood withdrawal via intravenous or arterial routes.
- Refraining from routine endotracheal suction.
- Providing additional interventions for pain or stress relief, such as non-nutritive sucking and administering breast milk or sucrose.
- Monitoring and Early Intervention: Regular cranial ultrasounds and head circumference measurements are essential for identifying PHVD and timely intervention.
Complications
IVH can lead to serious complications, including periventricular haemorrhagic infarction (PVHI), post-haemorrhagic ventricular dilation (PHVD), periventricular leukomalacia, and cerebellar haemorrhage.
Periventricular Haemorrhagic Infarction (PVHI):
PVHI typically occurs unilaterally, causing injury to corticothalamic pathways and disrupting neuronal and glial migration. This negatively impacts gray matter development. PVHI is associated with significant long-term complications: cerebral palsy in 60% of cases, cognitive impairments in 50%, visual field defects in 25%, and epilepsy in 20%. Mortality risk increases with the severity of the injury22,23.
Post-Haemorrhagic Ventricular Dilation (PHVD):
PHVD often develops 1–3 weeks after severe IVH, affecting approximately one-third of very-low-birth-weight preterm infants. Progressive hydrocephalus occurs in about half of these cases, with surgical intervention required in roughly 15%. Early detection is critical, and regular monitoring of head circumference is essential. An increase of more than 1 mm per day warrants further investigation to diagnose and manage PHVD effectively22.
Treatment
Currently, there is no definitive treatment for IVH. Management focuses on supportive care, including stabilising hemodynamic, ensuring adequate oxygenation and ventilation, providing appropriate fluid and nutritional support, controlling seizures, and addressing complications as they arise.
Prognosis
The prognosis for IVH depends on the severity of haemorrhage, the presence of parenchymal injury, and the occurrence of seizures or the need for shunt placement8,24. Infants with grade I-II IVH may experience neurodevelopmental delay, hearing loss, and cerebral palsy. In grade I IVH, cerebral palsy occurs in 6.8% of cases, and in grade II IVH, in 8.1%25. The incidence of cerebral palsy increases in the presence of ventricular dilatation or cystic periventricular leukomalacia. In grade III-IV IVH, cerebral palsy occurs in over 50% of cases, with 75% of children requiring special education. The incidence of severe neurodevelopmental disorders in grade IV IVH may exceed 55%, rising to 86% when PVHI and shunting are present22.
According to NICE guideline (NG72), comprehensive neurodevelopmental follow-up, including physical therapy, occupational therapy, and specialised educational support, is essential to optimize outcomes for affected infants.
Conclusion
Preventing and managing IVH in preterm infants requires an integrative approach spanning antenatal, perinatal, and postnatal care. Evidence-based strategies such as antenatal corticosteroids, delayed cord clamping, optimised ventilation, and neuroprotective bundles have proven effective in reducing IVH incidence and severity. Continued research into innovative therapies and long-term support systems is crucial to improving outcomes for this vulnerable population.

Aishlin Lok
Neonatal Consultant, Bradford Royal Infirmary
References
- van Beek PE, Groenendaal F, Broeders L, Dijk PH, Dijkman KP, van den Dungen FAM, et al. Survival and causes of death in extremely preterm infants in the Netherlands. Arch Dis Child Fetal Neonatal Ed. 2021;106:251–257. doi: 10.1136/archdischild-2020-318978.
- Christian EA, Jin DL, Attenello F, Wen T, Cen S, Mack WJ, et al. Trends in hospitalization of preterm infants with intraventricular hemorrhage and hydrocephalus in the United States, 2000-2010. J Neurosurg Pediatr. 2016;17:260–269. doi: 10.3171/2015.7.PEDS15140.
- de Figueiredo Vinagre LE, de Siqueira Caldas JP, Martins Marba ST, Procianoy RS, de Cassia Silveira R, Santiago Rego MA, et al. Temporal trends in intraventricular hemorrhage in preterm infants: a Brazilian multicenter cohort. Eur J Paediatr Neurol. 2022;39:65–73. doi: 10.1016/j.ejpn.2022.05.003.
- Bassan H. Intracranial hemorrhage in the preterm infant:understanding it, preventing it. Clin Perinatol. 2009;36:737–62. doi: 10.1016/j.clp.2009.07.014.
- Kooi EMW, Richter AE. Cerebral autoregulation in sick infants: current insights. Clin Perinatol. 2020;47:449–467. doi: 10.1016/j.clp.2020.05.003.
- Verma PK, Panerai RB, Rennie JM, Evans DH. Grading of cerebral autoregulation in preterm and term neonates. Pediatr Neurol. 2000;23:236–242. doi: 10.1016/s0887-8994(00)00184-3.
- Babnik J, Stucin-Gantar I, Kornhauser-Cerar L, Sinkovec J, Wraber B, Derganc M. Intrauterine inflammation and the onset of peri-intraventricular hemorrhage in premature infants. Biol Neonate. 2006;90:113–21. doi: 10.1159/000092070.
- Volpe JJ. Intracranial hemorrhage:germinal matrix –intraventricular hemorrhage of the premature infant. In: Volpe JJ, editor. Neurology of the newborn. 5th edition. Philadelphia: Elsevier; 2008. pp. 517–88.
- Lu H, Wang Q, Lu J, Zhang Q, Kumar P. Risk Factors for Intraventricular Hemorrhage in Preterm Infants Born at 34 Weeks of Gestation or Less Following Preterm Premature Rupture of Membranes. J Stroke Cerebrovasc Dis. 2016;25:807–12. doi: 10.1016/j.jstrokecerebrovasdis.2015.12.011.
- McGoldrick E, Stewart F, Parker R, Dalziel SR. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. Cochrane Database Syst Rev. 2020;12:CD004454. doi: 10.1002/14651858.CD004454.pub4.
- Helwich E, Rutkowska M, Bokiniec R, Gulczynska E, Hozejowski R. Intraventricular hemorrhage in premature infants with Respiratory Distress Syndrome treated with surfactant: incidence and risk factors in the prospective cohort study. Dev Period Med. 2017;21:328–335. doi: 10.34763/devperiodmed.20172104.328335.
- Wei JC, Catalano R, Profit J, Gould JB, Lee HC. Impact of antenatal steroids on intraventricular hemorrhage in very-low-birth weight infants. J Perinatol. 2016;36:352–356. doi: 10.1038/jp.2016.38.
- Hemmati F, Sharma D, Namavar Jahromi B, Salarian L, Farahbakhsh N. Delayed cord clamping for prevention of intraventricular hemorrhage in preterm neonates: a randomized control trial. J Matern Fetal Neonatal Med. 2022;35:3633–3639. doi: 10.1080/14767058.2020.1836148.
- Klingenberg C, Wheeler KI, McCallion N, Morley CJ, Davis PG. Volume-targeted versus pressure-limited ventilation in neonates. Cochrane Database Syst Rev. 2017;10:CD003666. doi: 10.1002/14651858.CD003666.pub4.
- Altaany D, Natarajan G, Gupta D, Zidan M, Chawla S. Severe intraventricular hemorrhage in extremely premature infants: are high carbon dioxide pressure or fluctuations the culprit? Am J Perinatol. 2015;32:839–844. doi: 10.1055/s-0034-1543950.
- Fabres J, Carlo WA, Phillips V, Howard G, Ambalavanan N. Both extremes of arterial carbonsdioxide pressure and the magnitude of fluctuations in arterial carbon dioxide pressure are associated with severe intraventricular hemorrhage in preterm infants. Pediatrics. 2007;119:299–305. doi: 10.1542/peds.2006-2434.
- Vesoulis ZA, Flower AA, Zanelli S, Rambhia A, Abubakar M, Whitehead HV, et al. Blood pressure extremes and severe IVH in preterm infants. Pediatr Res. 2020;87:69–73. doi: 10.1038/s41390-019-0585-3.
- Castrodale V, Rinehart S. The golden hour: improving the stabilization of the very low birth-weight infant. Adv Neonatal Care. 2014;14:9–14. doi: 10.1097/ANC.0b013e31828d0289. quiz 15-16.
- Kochan M, Leonardi B, Firestine A, McPadden J, Cobb D, Shah TA, et al. Elevated midline head positioning of extremely low birth weight infants: effects on cardiopulmonary function and the incidence of periventricular-intraventricular hemorrhage. J Perinatol. 2019;39:54–62. doi: 10.1038/s41372-018-0261-1.
- Hatfield LA, Murphy N, Karp K, Polomano RC. A systematic review of behavioral and environmental interventions for procedural pain management in preterm infants. J Pediatr Nurs. 2019;44:22–30. doi: 10.1016/j.pedn.2018.10.004.
- Shah V, Hodgson K, Seshia M, Dunn M, Schmolzer GM. Golden hour management practices for infants <32 weeks gestational age in Canada. Paediatr Child Health. 2018;23:e70–e76. doi: 10.1093/pch/pxx175.
- Adams-Chapman I, Hansen NI, Stoll BJ, Higgins R NICHD Research Network. Neurodevelopmental outcome of extremely low birth weight infants with posthemorrhagic hydrocephalus requiring shunt insertion. Pediatrics. 2008;121:e1167–77. doi: 10.1542/peds.2007-0423.
- Bassan H, Limperopoulos C, Visconti K, et al. Neurodevelopmental outcome in survivors of periventricular hemorrhagic infarction. Pediatrics. 2007;120:785–92. doi: 10.1542/peds.2007-0211.
- Brouwer AJ, Groenendaal F, Benders MJ, de Vries LS. Early and late complications of germinal matrix-intraventricular haemorrhage in the preterm infant:what is new? Neonatology. 2014;106:296–303. doi: 10.1159/000365127.
- Ancel PY, Livinec F, Larroque B, et al. Cerebral palsy among very preterm children in relation to gestational age and neonatal ultrasound abnormalities:the EPIPAGE cohort study. Pediatrics. 2006;117:828–35. doi: 10.1542/2005-0091.