On this page

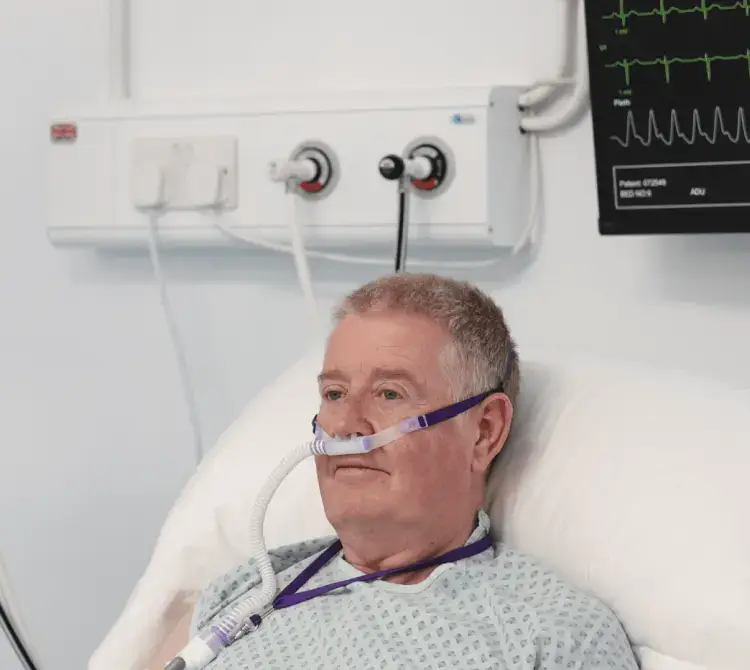
With such a busy environment in our Healthcare system, so many new staff and immense pressure on resources; saving time and cost are of the essence.
Humidifying patients can be a confusing phenomenon; learning how it works, when to apply it and what works best for each patient, alongside grasping the medical equipment needed for the treatment.
Let us explore humidification.
For both ventilated and non-invasive ventilated patients there are two options: active or passive humidification.
Absolute Humidity and Relative Humidity
Humidity refers to the quantity of water vapour in a gaseous environment [1] and is the process of increasing the moisture content of air, depending on the temperature of the gas. Humidity is expressed as absolute humidity and/or relative humidity. The absolute humidity (AH) is the amount of water in a given volume of gas, usually expressed in mg H2O/L volume [1,2]. The relative humidity (RH) is the amount of water vapor in a volume of gas, expressed as a percentage of the amount of water vapor required to fully saturate the same volume of gas at the same temperature and pressure [1].
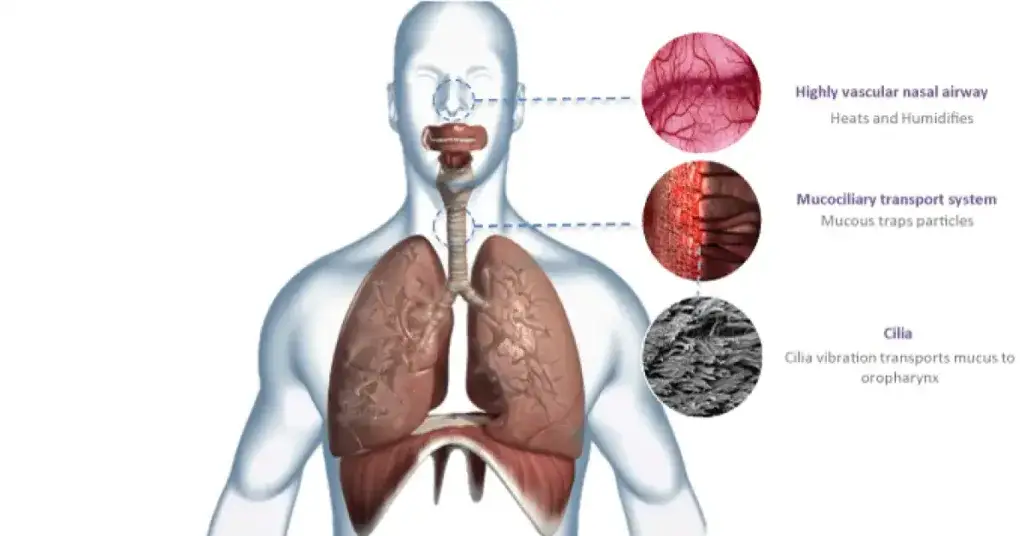
Our natural ability to humidify
During spontaneous breathing, the air entering the upper airways is heated, moistened and saturated naturally. At the carina, at normal body temperature (37°c), the absolute humidity is at 44mg H2O/L.
What happens when we artificially ventilate a patient?
When a patient is artificially ventilated with an ETT or a tracheostomy, these naturally occurring humidification mechanisms are bypassed, meaning that the patient’s natural ability to filter, humidify and warm inspired air are removed. This can result in increased and thickening of mucus secretions, ciliary function depression and therefore the cessation of the mucociliary transport, which can lead to an increased risk of infection, impaired secretion removal and atelectasis.
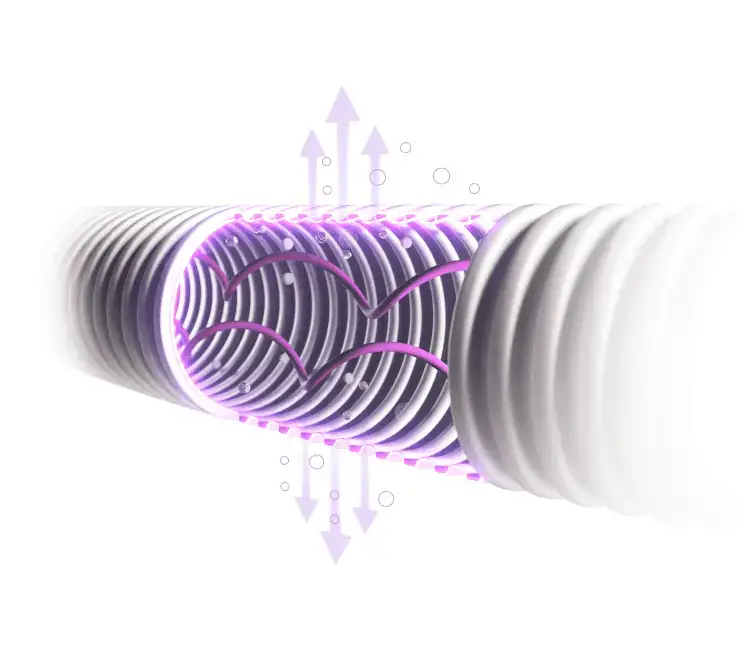
Passive humidifcation - HMEs
An HME (heat and moisture exchanger) filter can be placed in the circuitry to the patient. HMEs retain some of the patient’s own exhaled heat and moisture and use this to heat and moisten the next inhaled breath, therefore replicating the body’s natural ability to heat and moisten air. HMEs can be hydrophobic or hydroscopic and can increase the resistance to airflow, not only during inspiration, but during expiration. Although it may seem quicker and easier to set up, HMEs increase dead space, some more than others, notably having greater effect on children than adults. This increase in dead space decreases alveolar ventilation and raises PaCO2. Some issues can arise with HME filters; they can become clogged with fluids or secretions, causing potential further issues if not changed regularly and add weight to the circuitry, increasing the risk of tube dislodgment. However, when it comes to transporting the patient, they appear to be the most popular choice.
Active Humidification
Active humification use devices that add water molecules, gas and temperature. There are various types of set up but the most common are the ‘water bath’ based passover type. With passover humidification, a water chamber is placed on to a heater plate, a bag of sterile water feeds water into the chamber to create the vapour and the gas going to the patient picks up the moisture and warmth and transports it to the patient through the heated wire circuit. This is aided with cables attached to both a heated circuit and to the chamber/humidifier, ensuring the patient receives optimised heated gases quickly and effectively.
Choosing Active or Passive Humidifcation?
We know that decisions regarding active or passive humidification will remain on the cards for many years to come but it is important to remember the fundamental benefits of delivering humidification (in whatever method) to patients requiring respiratory support.
If we look at the anatomy of our bodies, and in particular our lungs, performing all the wonderful jobs they are designed to do; they are truly amazing.