Breathing Easier: What Non-Invasive Respiratory Support Can Mean for NICU Parents
- Published on:
Breathing Easier: What Non-Invasive Respiratory Support Can Mean for NICU Parents
- Published on:

On this page

Introduction
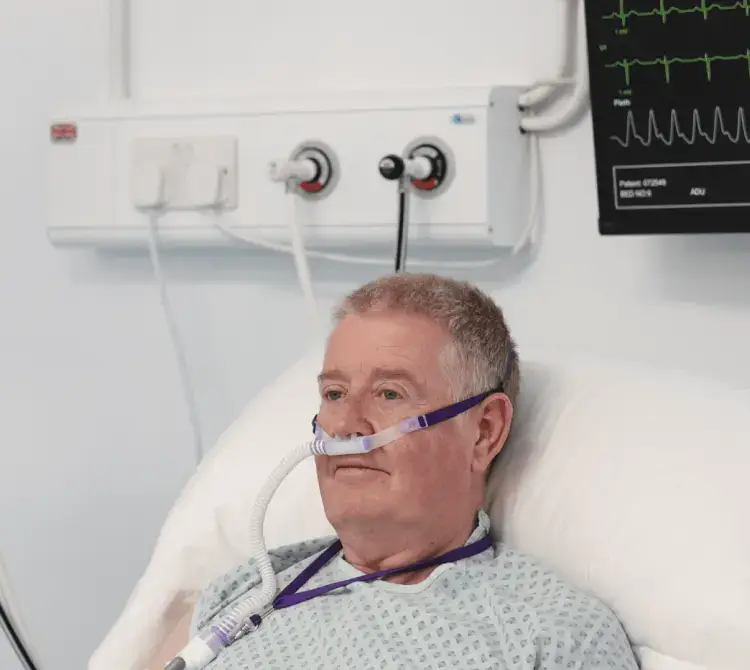
When my baby was born at 31 weeks, I entered a world I didn’t know existed. I wasn’t prepared. No one had told me what to expect and I was finding my feet on how to be a Mum, when I felt I was wading through a fog of trauma. When I first met my baby, I didn’t know which one he was. I looked around the room covered in incubators and searched for him. I wouldn’t have known if I was on my own and I held a guilt for that. When I first saw him, he was covered head to toe in wires, tubes and masks. There were beeps and blue lights. I was in a wheelchair, unable to stand and see him properly through the incubator doors. A nurse asked, “Does he have a name?”, to which I looked shocked and unsure. “A name?” I thought; I can’t even see his face. I don’t know what he looks like, how can he have a name? It took me time to name him, to see his face, to take in what had happened, to connect to him and what I had been through. It wasn’t until the masks and tubes started to be taken away that I was able to look at him and know his name.
When I came home, the NICU experience didn’t leave me and to be honest, I think it was when the gravity of what I had been through hit me. I reached out for support but couldn’t find it: either through the NHS or online. I wanted to find other people talking about how I was feeling, searching for validation. I was a Clinical Psychologist and I knew that others would be searching for this support too. Online, I met another Mum who had her baby at 31 weeks. We connected over shared experiences and decided to create a space where parents could feel heard, seen and validated. We called it Miracle Moon. Since that point, we have supported hundreds of families through NICU and beyond, through social media, our podcast, 1-1 support and our membership, The NICU Space.
Something that is spoken about within our community is the impact of your child being covered in masks, tubes, intubated. I have read papers about the benefits of non-invasive respiratory support for neonates, which are good clinical reads. But, as someone who spends every day listening to parents living it, remembering the trauma of their journeys, I wanted to explore what non-invasive respiratory support really means from a parent’s perspective – not just in outcomes, but emotionally.
The machines that add breath, but takes away from the connection
When parents enter the therapy room, they don’t talk about CPAP or ventilation in technical terms. They say things like:
Invasive intervention, even though lifesaving, can feel like a physical and emotional barrier between you and your baby. It is the moment you realise just how serious things are: seeing a machine breathing for your baby, keeping your baby alive. It is terrifying and can leave you feeling helpless and disconnected. A parent’s brain is primed for connection, so when those connection cues are blocked by intervention, it can feel like part of your role has been suspended and it can influence the bonding and attachment process for some parents. There is also a very real grief that parents experience – this is not how it was meant to be, this is not what they were expecting, and it can take time to accept that this is their reality.
Non-invasive support can still feel like a lot, but emotionally, it is often a turning point for parents. They may tell me things like:
These are big moments, they feel like connecting, bonding, reducing fear and allowing hope to seep in.
Closeness and control in an environment that takes both
Non-invasive support means fewer tubes, wires, more chances for holding, bonding, connection, which makes parents feel more like, well, parents.
Parents in our NICU Space community often say that they feel like they don’t know how to parent. They imagined being able to hold when they want, to cuddle and feed; but instead they have to wait, ask and hold their breath as their baby is being transferred – feeling terrified that they are going to stop breathing. They want to hold, change nappies, comfort their baby, take the lead. When the machines allow them to do that, it is more than a milestone, it feels like your identity is being handed back.
There’s a psychological shift from helplessness to agency. Small moments of control, like changing a nappy, being able to initiate a cuddle help to support a parents sense of self and reduce trauma related powerlessness. All of those ordinary acts of parenting become extraordinary in the NICU. It allows parents to build trust in themselves and their baby.
The nurses who say things like “Let me explain what is happening”, “Let’s make sure you get as many cuddles as possible”, “You can talk to them, read to them, touch them”, “Come closer, we’re here to help” makes all the difference. It’s not just the machines that help, it is how staff help parents to feel safe around them.
A practical step that feels like progress
From a psychological perspective, when we see our babies progress, even in small signs, it allows us to hold onto a bit more hope. It allows us to imagine that things could change, that there may be an end in sight. It helps parents to feel safer, to help regulate more in their trauma responses, there is a shift from crisis mode to cautious hope. For some, it may be the first time they let themselves breathe.
You allow yourself to imagine the next hour, the next day. You start to trust your baby’s strength. You start asking more about kangaroo care, breastfeeding, how you can help your baby, coming home, not just a frozen surviving.
What I wish professionals knew
I know that staff in neonatal care are juggling a huge amount – you are saving lives, every day. Having to be “on” and putting everyone else first. But parents are often holding something so heavy that they do not feel able to communicate, so I want you to know:
If you are a parent reading this
If you are sitting in NICU now, with your baby on breathing support, or a parent who has been there before, I want you to know you are doing a brilliant job. You have not failed. You are parenting in the most difficult circumstances, the machines do not define your baby, the disconnect does not define your relationship. You can both heal, you can both bond, it just may look a little different to what you imagined.
Every time you show up, no matter how scary it feels. Every time you talk to your baby, touch them, think of them, every time you sit by their side, you are showing up with more love and courage than most people ever have to give.
At the NICU Space and Miracle Moon, we offer support for parents just like you. Whether you are in NICU now or processing what has happened after coming home, we are here to support you through every step and connect you with other people who really, truly get it.
We believe that NICU parents deserve to be seen, not just as parents of the baby in neonatal care, but as vital, central figures in it.

Dr Frankie Harrison
Clinical Psychologist and NICU Parent
Co-founder, Miracle Moon